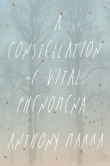
Текст книги "The Nurses: A Year of Secrets, Drama, and Miracles with the Heroes of the Hospital"
Автор книги: Alexandra Robbins
Жанры:
Прочая проза
,сообщить о нарушении
Текущая страница: 2 (всего у книги 33 страниц)
Later that morning, Priscilla gathered the ER nurses to tell them about the new uniform policy. While the group splintered into side conversations, Priscilla brushed her dark bangs off her face and put a hand on Molly’s arm. “I got your message,” she said.
“This place is coming apart at the seams,” Molly told her.
“I know.”
“I’m holding to my word on my message yesterday.”
Priscilla nodded, placating.
“I’m not changing my mind,” Molly said. “I’m giving you one month’s notice. The uniform is just the last straw.” She could call the agency tonight, start the re-registering process, and begin orientation within weeks. She was giving Pines Memorial ample notice because she didn’t want to leave her coworkers even more shorthanded.
Throughout the rest of the day, nurses complained about the policy. “They’re kicking us when we’re down,” they said. “The changes are making things worse.” They looked at Molly because she was one of the most outspoken nurses.
“Doesn’t matter to me,” she said. “I just quit.” Her coworkers laughed dismissively. “No, I actually did, y’all. I gave notice.”
Generally, Pines Memorial’s schedules were flexible and fair, and Molly had come to value the nurses’ intelligence and ability to stay cool under pressure. But, she thought, I can’t be angry at work every single day.
Molly had originally decided to make the career switch from occupational therapy to nursing after her mother had passed away. While in mourning, Molly received several letters from her mothers’ coworkers. The letters “talked about her being the best nurse they had ever known, how much fun she made work, and how much the patients and her coworkers respected her,” Molly remembered. Inspired, Molly became a nurse, too, at the age of 27—ten years ago. “I’m not that touchy-feely, but I truly love nursing. It’s a meaningful career, I’m good at it, and it’s flexible,” she said. “You can find work any time of day, any day of the year, which makes it mom-friendly.”
Molly had wanted to be a mom for as long as she could remember. After three years of trying to conceive with her police officer husband, Trey, she had finally scheduled an appointment at a fertility clinic. As an agency nurse, she would be able to arrange her schedule around her clinic appointments.
More experienced colleagues kept telling Molly that once she worked at several other hospitals, she would realize that Pines wasn’t that bad. “Will I find out from working at other places that that was really as good as it gets?” she wondered. Experiencing hospital life at various institutions was the best way Molly could discover whether anybody was treating both nurses and patients right.
She gave herself a year to find out.
LARA
SOUTH GENERAL HOSPITAL, August
On her way to the staff locker room, Lara stopped in her tracks. The half-used vial of Dilaudid, a narcotic five to ten times more powerful than morphine, lay on a counter. It seemed to shimmer with energy and promise. You deserve it, coaxed a voice she remembered well. You’ve been working fourteen-hour days. Your mom just died. She died in your arms. It will make you feel better. It’s sitting right there. No one will know. You want it. Take it.
Lara had been a drug addict. It had started so innocently. Nine years ago, as a single 26-year-old nurse, Lara was chatting with the other nurses on the night shift about paying off school loans, when one of them said, “Did you know you can get four thousand dollars per egg if you donate them? We should all go together.”
“That’s kind of cool,” Lara had said. “I’m young, I’m healthy, and it’s easy money.”
The next morning, the four nurses went to a clinic for the screening process. Lara, with her blonde ringlets and fair skin, was the only donor selected. After the multi-week process of egg retrieval, the doctor handed her a check and a prescription for Percocet.
The pill was the first narcotic she had ever taken. Within minutes, she was simultaneously giddy and calm, suffused with warm happiness, the world’s best buzz. She couldn’t stop giggling. Nothing bugged her. Her insecurities—about her dating life and her skinny boy’s body, which was never fit enough for her standards—dissolved. The next day, she took another pill. She didn’t think twice about it. It was her prescription, it energized her, and there were no side effects.
At work she was chattier and also more mellow than usual, and she managed to stay cheerful even while dealing with ungrateful patients and tedious charting. She skipped lunch breaks. When she finished the pills, a girlfriend who didn’t need her prescription anymore offered the pills to Lara. Why not? Lara thought. That week, she took three pills at a time.
A few days after the bottle emptied, Lara started to feel sick. That afternoon at work, she remembered that she had morphine in her pocket, 1 milligram left over from a patient. Back then, hospitals weren’t as vigilant about counting the “waste”—the surplus drugs left over from patients’ prescribed doses. Nurses went home, shrugged off their scrubs, and dumped their pocket contents into the trash.
She fingered the vial, running her thumb along the smooth, cool glass. If the Percocet made me feel that good, maybe morphine will, too, she thought. She returned it to her pocket to use at home. There was no inner voice asking her what she was doing, no angel on her shoulder imploring for restraint. It was just a little shot in the arm to take the edge off the day. She would never actually take narcotics at work, she told herself.
For the next several months, Lara conveniently “forgot to waste” leftover narcotics. Instead, she brought them home and stashed the Percocet, morphine, or Dilaudid in her underwear drawer. In the beginning, the drugs popped into her mind only occasionally, an elated realization like finding a twenty-dollar bill at the bottom of a purse: Oh! I have extra narcs in my pocket! She brought home vials about twice a week. It was too easy. Even once her hospital began requiring nurses to dispose of the excess in front of a colleague, the drugs were there for the taking. “Hey, I’m wasting this milligram of Dilaudid,” Lara would say, and the nearest nurse would hardly look up as she scribbled a signature. No one bothered to watch whether Lara actually threw out the vial, a procedure intended to prevent exactly what Lara was doing.
Not only was she able to do her job while taking the drugs, but she also had more energy than she knew what to do with. She worked additional hours for overtime pay. She justified the drug use by telling herself that her increased energy made her a more productive nurse. “You’ve heard about soccer moms being able to do everything on Ritalin? That was me. I could work! I could do ten thousand things and no one suspected why.”
Within months, Lara’s tolerance increased and her main concern at the hospital became collecting more drugs to bring home. One milligram wasn’t enough to spark a buzz, and she felt fatigued if she tried to go more than a day without taking something. So she signed up to work every day—zero days off—to get access to the meds because she didn’t want to feel tired. She was often sick to her stomach, but didn’t make the connection between her stomachaches and the drugs.
If you had asked Lara before she donated eggs what she thought about people who took narcotics, she would have responded, “Why on earth would someone do that?” Now it did not occur to her that she had become one of those people. It didn’t even occur to her that she was doing drugs (as opposed to taking medicine), let alone stealing them.
Lara was a superstar nurse, energetic without being perky, unfailingly positive, and constantly volunteering to help other nurses. Nobody questioned her, nobody told her it wasn’t healthy to work seven days a week. There was always a need for more hands. She would call the nurse manager and ask nonchalantly, “Hey, can I come in for four hours this afternoon?” Nobody ever said no.
About a year after she took her first Percocet, the workday started to seem longer. Lara was eager to get home so that she could inject herself. The first time she shot up in a staff bathroom, a voice broke through her thoughts: “It’s getting bad if you can’t even wait to get home.” I have a hard job and it’s a long day, she told herself. If other people saw what I see at work, they’d need something to take the edge off, too. “You’ve crossed the line you drew for yourself.” I can stop at any time.
Lara took sixteen-hour shifts, sailing through them with midday bathroom breaks to insert an IV, eventually injecting up to 8 milligrams of Dilaudid at a time, an enormous dose, but, for Lara, just enough to keep her alert. Once, she put a heparin lock in her foot to give her quicker access to a vein. She wore it the entire workday, attending meetings and caring for patients. She told coworkers she was limping because she had dropped a weight on her toes.
Because the medications helped her to excel at her job and to work extended hours, Lara didn’t admit to herself that what she was doing was dangerous.
One afternoon, she realized that she hadn’t wasted a single narcotic in five consecutive workdays. Somehow, over the past several months, her maneuvers had shifted from secretive to sloppy. Surely, she worried, someone would catch on to her. She took a swig of Pepto-Bismol to calm her stomach, which was shaky as usual. She blamed her nerves, because she was applying for a position as a flight nurse on a medical trauma helicopter, her ultimate career goal since nursing school. Ugh, if I could just get another vial, then I won’t feel sick. Then it hit her. Oh my God, it’s not because I’m nervous. It had taken her that long to see, or accept, the link between her stomachaches and her addiction.
Many addicts say that there is often no single defining event that leads them to want to stop using. For some, there simply comes a point when they are ready to admit to themselves that they have a problem and they don’t want to have that problem anymore. That’s how it was for Lara. That day was no different from the day before, except that a layer of her denial suddenly lifted. Later, she would be amazed that she had ignored the signs of addiction for so long.
Once it clicked, she was petrified. She was ashamed of herself and afraid of what people would think; she didn’t know which was worse. She vowed to do everything she could to quit her addiction. Lara tried calling in sick to force herself into withdrawal. Okay, I kicked this. It’s cool, she would say to herself after a few days. But then she would return to the hospital to find that her desire for the drug was stronger than she was. After hours of trying to tough it out, she would grab a vial and a needle, so easy, so irresistible, and run to the bathroom.
She attempted to discourage herself by calling her brother, whom she didn’t want to disappoint. She wrote herself letters: “This isn’t how you want to live your life.” She tried stipulating that she could shoot up only at night to help her sleep, or she could use only morphine so she wouldn’t get as sick. She told her roommate, Angie, a fellow ER nurse she loved, so that someone else could hold her accountable. Lara and Angie had been ER nurses together for six years. Angie was the type of strong nurse that other nurses wanted in the room with them. When they started out as new nurses together, they had leaned on each other to endure the ER sink-or-swim craziness the way many nurses did if they were lucky enough to find a competent, likeable partner. Lara and Angie had combined their strengths and pulled each other through stints at two hospitals.
Angie could not believe it. She was sympathetic but appalled. She wouldn’t turn Lara in, yet couldn’t persuade her to stop using for long. Each time Lara tried to stop, within twenty-four hours she slid from being able to glide through her shift and an invigorating workout at the gym to feeling too sick and depressed to function. She felt like she had the worst flu possible, a debilitating illness that could vanish in moments after an injection. So she kept injecting. She didn’t know that there were narcotics addiction treatment programs specifically for medical professionals. She didn’t know what else to do. I need to stop feeling so sick, she told herself. I’ll take something today and then I’ll stop tomorrow. She said this for four more months.
Eighteen months after her first Percocet, Lara was offered the dream job that she had applied for: a flight nurse for a hospital system. Flight nurse opportunities, prestigious within the field, were rare. When Lara saw the helicopter she would be working on, she couldn’t contain her exhilaration. She ran her hand along the airframe, climbed inside, and sat in the nurse’s seat, incredulous that she was exactly where she wanted to be.
The next day was a Thursday. Determined to get clean, Lara checked into the drug treatment program at her hospital. She thought she simply needed to get over a few days of drug withdrawal. She’d let the professionals get her clean over the weekend, and she’d leave on Monday, the drugs gone from her system, her body free from their grasp. Lara assumed her hospital was so large that no one would see her. She didn’t turn herself in to her ER bosses because she figured she would quickly get this sorted out. Still in some measure of denial, Lara thought that she could conquer any treatment plan they gave her. After all, she was strong. She was determined. She still didn’t realize she was that sick.
That weekend, when Lara was feverish from narcotics withdrawal, Angie called from the ER. The director told Angie that the department had been aware of Lara’s problem for months. “The ER knows what’s going on,” Angie said. “They know you’re stealing drugs and I think you should turn yourself in.”
I’m an idiot, Lara thought. Who goes in for drug treatment at the same hospital where they work? She raced to turn herself in, hoping the consequences would be lighter if she admitted she had a problem and was desperate for help. She dashed out of the building and down the sidewalk in the sweatpants she’d worn for two days straight and a long-sleeved shirt covering the marks on her arms that she didn’t want anyone to see. She sprinted the block between the treatment center and the ER and barreled into the director’s office.
Before the ER director had a chance to speak, Lara unloaded. “I have a problem and I can’t stop and I’m trying to get help and I’m in treatment now,” she blurted through tears. “I don’t want to live like this anymore.”
The director had been one of Lara’s favorite people to work with. A former nurse, she came into the unit and helped when the staff was overburdened. Unlike Lara’s previous administrators, who would either sit comfortably in their back offices while their nurses drowned in work or stand imperiously on the floor telling staff what not to do, this director rolled up her sleeves, pushed stretchers, and ordered food for her employees.
The director reluctantly pushed a large stack of papers across her desk. The file documented instances when Lara had taken narcotics under a patient’s name. Lara had never taken medications from a patient, but she had taken larger vials than patients needed in order to increase the leftovers. The administration had tracked her for approximately eight months.
“You’re under investigation,” the director told her sadly. “We’re going to have to fire you. For a long time, I didn’t do anything because I just couldn’t believe it.”
Lara was scared. She didn’t know what would happen next. Would she go to jail? At the same time, she felt a tremendous sense of relief. This is over now and I can move on, she thought. Whatever happens is going to be better than where I’ve been. Now that it’s in the open, I don’t have to fight this battle by myself anymore.
Lara never found out why administrators didn’t report her to law enforcement. Perhaps it was because she had voluntarily turned herself in and had entered a drug treatment program. Or perhaps they didn’t want to derail the career of an exceptional nurse. Lara reported herself to state nursing board officials, who said that to keep her license, she would have to enroll in the Medical Drug Intervention program.
MDI (a pseudonym—most states have their own program) was an intense multiyear program designed to help nurses and other health professionals. Even after the initial thirty-day rehabilitation, patients were not allowed to work in any medical field, so they could focus exclusively on getting clean. MDI administrators decided when to allow a nurse to take a job. Lara met nurses who had been kept out of work for a year.
The thirty-day rehab program was a beast. Lara was the sickest she’d ever been. She had flu symptoms, sweats, chills, extreme fatigue, aches, and unimaginable joint pain. She couldn’t brush her teeth because it hurt too much to close her fist around her toothbrush. For weeks, the agony was unrelenting, but Lara was determined to take no medications to ease her through it. She attended her assigned meetings and classes, where program leaders introduced her to Narcotics Anonymous and forced her to examine her demons.
Lara didn’t need a therapist to explain to her why the drugs were so tempting. Her divorced parents had been physically and mentally abusive. She remembered vividly the days she arrived at school bruised from beatings, and the times her parents called her fat, ugly, and stupid or told her she would “never be smart enough to be a nurse.” Her mother was a mean drunk by night and a sweet woman by day, with no memory of her behavior the night before.
The program also taught Lara that she had been turning to narcotics to escape something else. Lara had believed she was strong enough to ably manage the horrors she saw in the ER—the dying babies, the grisly traumas. Her hospital allowed no time for debriefing; following a tragedy, nurses were expected to get right back to work. Lara had been repressing these images and experiences for years. She hadn’t realized they were eating away at her still.
Three months after Lara completed rehab, MDI placed her in a medical advice job. She had gone from working as a Level-1 trauma center nurse to answering an advice hotline. Mortified, she cried during her drive to work for the first two weeks. Every morning before 8 a.m., seven days a week, Lara had to call a 1-800 number to check whether she would be randomly tested. On testing days, within two hours of the call, she had to give a urine sample at a lab (and pay $55 for the test). If she missed the test, she would be kicked out of the program and lose her license permanently, no excuses.
Lara had slogged through the misery of withdrawal. She regularly called her case manager to complain. “I hate you guys!” she’d say. “I’m not doing this. You can take my license.” Ten minutes later, she would call back, contrite. “No, never mind! I didn’t mean it!”
The program was so strict that Lara met many fantastic nurses who gave up their licenses rather than stick with it. But she was determined to tough it out. “MDI will back you up when you reapply for your license. They want to know how serious you are,” she explained. “Now that I can look back, they did know what was best for me when I didn’t. I wanted to go back to the ER. But they had to approve the job.”
After two years, MDI allowed Lara to resume patient interaction by working at a doctor’s office for eighteen months. Finally, MDI let her interview for an ER job at a different hospital. Her résumé was still impressive. She breezed through the interview until the end, when she was required to mention the program. Every month, her employer would have to fill out forms asserting that Lara was not impaired at work.
Another nurse in the program had given Lara advice: “Just look them straight in the face and say, ‘I’m doing the right thing now, and have been for a long time.’ Don’t apologize. You made a mistake. You’re moving on.” So she did, unflinchingly looking the interviewer in the eye.
“I’m impressed that you’re so honest with me,” the interviewer said. She told Lara later that she gave her the job because she was so forthright.
Lara had done so well with her recovery that her mother asked her to take her to an AA meeting. Her mother never drank again. Soon, her brother made the same request. Before long, Lara’s family was sober. But Lara’s battle wasn’t over; it probably would never truly end.
After twelve months in the ER position, Lara was considered an official graduate of the program. She would not have to disclose her drug issue or treatment again.
Years later, when she applied for the job at South General Hospital, she didn’t mention the addiction. She considered herself fortunate for many reasons, one of them being that the coworkers and friends she did tell about her addiction didn’t judge her. She felt secure knowing that her friends, including Angie from one ER and Molly and Juliette from another, were supportive.
One of the great aspects of nursing was that it could forge lasting bonds. Working so closely with coworkers on matters intimate and important created the kinds of forever friendships that could buoy a nurse through long hospital days. Molly, a straight shooter, and Juliette, a loyal pal, fell into that category. “When nurses get to know each other, we have each other’s back. We really will do anything for each other,” said Lara, who worked every Christmas holiday shift for thirteen years straight before she had kids so that other nurses could celebrate with their children.
Despite the facts that nine years had passed since her first Percocet and Lara was married now with two beautiful children, at South General narcotics tempted her every day. There were even more drugs available here than at her first ER. Nurses constantly left half-full vials on the counters and the protocol for disposing of them was often ignored. Oh, look at that, there are some narcotics sitting right there, a little voice would nudge Lara.
She knew that the relapse rate for narcotics addiction was extremely high. To keep herself in check, she attended three Narcotics Anonymous meetings a week. She could count on dozens of friends she had made through NA who would help in an emergency. “In a way the addiction is a huge blessing because I have real strong people in my life now and they help me,” Lara explained. “I would have never thought that such a horrible situation would turn so positive.”
Lara had been doing pretty well resisting temptation, all things considered. Until six days ago, when her mom, long suffering from emphysema, died in her arms. She was 65. Lara was devastated. She didn’t know how to cope with the loss of a parent.
Now, on her first day back at work since the funeral, Lara stared at the vial in front of her. The narcotic promised her security, comfort, confidence, and a happy buzz that would dull the pain of her mother’s death. She wanted it so badly she could barely breathe. It will make you feel better. No one will know. You want it. You deserve it. Take it.